Colorado Crisis Care
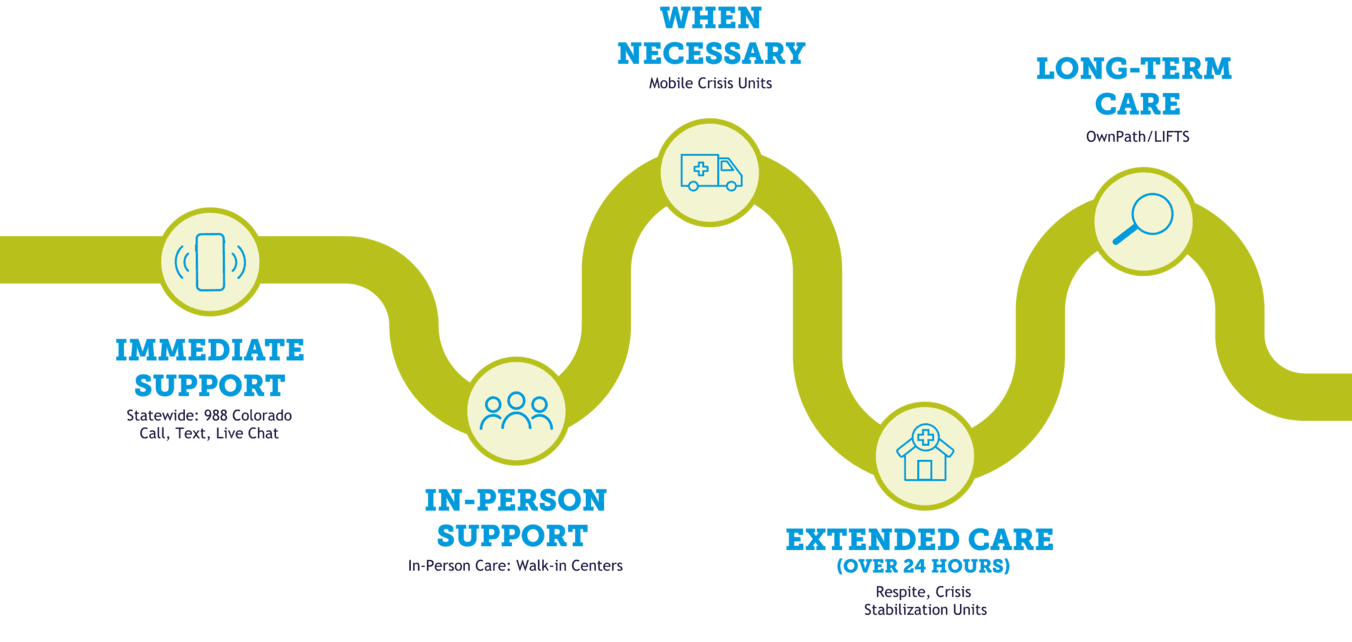
The Colorado Crisis System is Here for You
Whatever you're going through, there's meaningful support available 24/7. Let's go through the different options available.

Immediate support line
988 Colorado Mental Health Line
988 is the easy-to-remember number that allows anyone with emotional, mental health, or substance use concerns to be immediately connected with a trained specialist who will listen without judgement. 988 Colorado is free, confidential, and available 24/7.
If you or someone you know is struggling, needs peer support, call or text 988 or live chat at 988Colorado.com.
Walk-in Centers
Walk-In Centers (WICs) are available 24/7/365. They offer help in person if you are having a mental health crisis. Crisis professionals are available to meet with you. They can offer support and help you make a plan for care. WICs do not have beds for overnight stays. If you need more than 23 hours of help, they will identify another place that can help. Find a Walk-in Center near you.

Mobile crisis response
Mobile Crisis Response (MCR) is a program that provides face-to-face support to individuals experiencing a self-defined crisis. When MCR teams are dispatched by 988 Colorado Mental Health Line, crisis professionals will arrive at an individual’s location, assess and de-escalate the situation, and arrange follow-up care if necessary.
Mobile crisis teams do not include law enforcement, and the 988 Colorado team will help determine the appropriate intervention for the help seeker. If you need immediate mobile response services, call/text 988 or live chat at 988Colorado.com.
Crisis stabilization units
Crisis Stabilization Units (CSUs) offer short-term care for youth and adults experiencing an urgent behavioral health crisis. CSUs are not hospitals, but are staffed by caring and trained providers who can provide assessment, therapy, peer support, psychiatry, and coordination of ongoing treatment. CSUs offer 24-hour care for a short period of time.
Find a CSU near you by visiting OwnPath Care Directory.
Respite services
Respite services are available 24/7/365 and provide temporary or short-term crisis intervention for children, youth, adult, or family caregivers intended to mitigate an immediate crisis. Intervention is intended to stabilize the crisis while providing clinical interventions and formally developing ongoing care planning and case-management services that an individual needs. Respite services can be performed in residential or community-based settings based on individual need.
Find a respite service near you by visiting OwnPath Care Directory.
Colorado LIFTS
It isn’t always easy to know where to start or how to get the right support. That’s where Colorado LIFTS (Linking Individuals and Families to Services) come in. Colorado LIFTS’ helps make behavioral health services more accessible, affordable, and easier to navigate—so Colorado residents can get the care they need for whole-person health.
Access Colorado LIFTS care navigation and providers by visiting ownpath.co to search for BHA-licensed providers in your area.